
Do you have ganglionic cyst?
Ganglion cysts are swellings of fluid on top of foot joints such as the big toe joint, the top of the foot and the ankle. A cyst by definition is a sac filled with fluid and it can feel hard or soft. Ganglionic cysts of the foot, wrists or hands are usually not dangerous and they usually occur between the ages of 20-40 years of age.Most common locations of a ganglion cyst
-
Where the fingers and the hand meet.
- The tips of the fingernails and toenails- this is called a mucous cutaneous cyst ( Mucous Cyst)
- The outside of the knee
- The outside of the ankle
- The top of the foot
- The big toe joint
Cause of ganglionic cysts
Ganglionic cysts can be though of as a protrusion of fluid from a joint that is still surrounded by a sac of membranous tissue. Think of this like squeezing a water balloon with your hands in all areas except a small pocket, that area of the balloon with pouch outward- this is what is happening with your joint. A thin canal of fluid forms and pouches outside the joint.Ganglionic cyst symptoms
- If feels like a bump that can be soft or hard.
- It should not move as you push on it
- The size may increase or decrease depending on if you elevate or lower your hands and feet over time (but this is not always consistent)
- Most of ganglionic cysts can cause pain, especially the ones around your toenail.
- Pain can be the worse around the joint
Home treatment of a ganglionic cyst
See a Podiatrist even if it doesn’t hurt. Even though a ganglionic cyst is usually harmless except for the pain, there is always a chance that this could be a cancerous tumor such as a synovial sarcoma(very low odds).- The ganglionic cyst has the nickname “Bible Cyst” because hitting the cyst really hard with a bible made it go back temporarily, but this ganglion cyst will almost always eventually come back. The only true cure is to have your podiatrist perform a ganglion cyst removal surgery.
Podiatrist treatment of a ganglion cyst
- X-ray is essential to rule out other types of tumors- Don’t mess around with this one, make sure its actually a ganglionic cyst.
- Ultrasound will confirm that the mass is fluid filled.
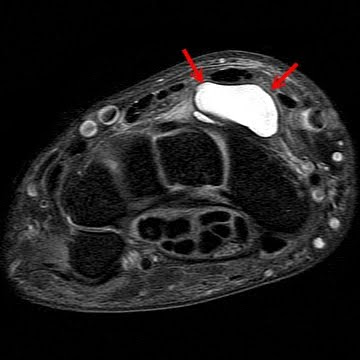
- MRI can also be ordered if there is difficulty confirming the mass with an ultrasound, although this is rarely necessary.
- A podiatrist can perform aspiration of the ganglion cyst in the foot.
What to expect after the aspiration of a ganglion cyst in the foot?
After the aspiration of the ganglion cyst, you will likely be free of the ganglionic cyst for some time; but eventually it is almost guaranteed to come back. The only true cure for a ganglion cyst in the foot is aspiration.Ganglionic cyst removal surgery by a podiatrist
- The only way to keep a large ganglionic cyst from removal is excision- The healing time is usually very good as the incision is usually not from the bottom of the foot and you can start walking immediately after the ganglion cyst removal surgery
- You will likely need to wear a bandage for at least 7-10 days and maybe a surgical shoe to prevent irritation of the wound.
Ganglionic foot cyst removal surgery recovery time
The recovery time depends on a variety of factors, but if it is on the top of the foot(which it almost is), you can start walking almost immediately and take the sutures out in about 2 weeks.To learn more about ganglionic foot cyst and treatment options see this link.

